Boehm 10
September 2002
Frank Boehm
Frank Boehm
None
The Gastrointestinal Micro Scanning Device (GMSD) would be a stand-alone device and system in its own right, however it also would serve as an interim application (involving similar technology) of the Vascular Cartographic Scanning Nanodevice (VCSN). The GMSD system would be nearer term and more macro-scale as it would be scanning the digestive tract, a larger and far more straightforward system to scan. The scanning Emitter/Receiver units for this setup might utilize a concentration of some type of quantum dot laser nested with a receiver/timing unit.
The GMSD system would consist of three separate components working in unison to generate a very high-resolution 3D topography of the entire internal surface of the gastrointestinal tract (GIT). It would accomplish this task by employing:
1. An internalized scanning device (Bright Ball) (BB).
2. A pulse generator/data transfer unit (PGDT).
3. A pixel matrix software, and display element.
This scanning device would be spherical in shape and ~3 mm in diameter. (An assessment would be done to ascertain the optimal physical parameters for the device to eliminate the possibility of the BB getting “snagged” en route). It would consist of an array of emitter/receiver (ER) units, which would be ~1 micron in diameter and would abut with several thousand other units to make up most of the exterior spherical surface. Each unit would be set in place and bonded with some type of biocompatible and biodegradable material. This material would encapsulate all of the ER units to make up a solid sphere, which would have a highly polished finish.
Every ER unit would be a separate and distinct measuring device. The emitter would be a (as yet to be determined) species of laser. The receiver would be made of a laser sensitive material nested in close proximity to the emitter and would receive the reflected beam of the emitter from the target.
The ER units would be calibrated beforehand. Distance measurements of the internal topography of the GIT would be taken using time-of-flight calculations and would be arrived at via inference to the initial reference calibration.
The pulse generator/data transfer unit is the component that would trigger the internalized BB device with an appropriate signal. The BB can be activated to scan by this specific signal only. Once activated, it would emanate a constant data stream to the PGDT. The PGDT will act as the data transfer vehicle when linked to a computer and the Pixel Matrix software. It will be affixed to an appropriate area of the patient’s abdomen and will stay in place for the duration of the scan.
The pixel matrix software would take the data supplied to it by the PGDT and construct a 3D rendering of the total scanned area traveled by the BB. The software would also have a “fly-through” and cross-sectional capabilities allowing the physician (using a joystick or computer mouse with the display) to move through the entire GIT to investigate any potential problem areas. One can envision a time when this digitized information could be translated into a holographic rendering as well. The physician would be able to recognize topography consistent with tumor growth, lesions, and other abnormal features that may exist in the tract using this procedure.
The set-up for the GMSD operational procedure would be simple to implement. Firstly, the BB would be administered orally to the patient by the same method used to take any pill. Next the PGDT patch would be affixed to the patients abdominal wall. At this point an equipment test would be performed to assure that the communications link between the BB and the PGDT is functioning properly. A test scan would also be done to configure the image resolution. The patient can then leave the office and go about their normal routine.
The BB, now internalized, would move along with the natural rhythms of the GIT and would be eliminated naturally at the end of the transit duration. The patient would return to the facility in two or three days (depending on the assessed GIT transit time) to have the PGDT patch removed.
The PGDT would now contain all of the positional data emanated by the BB during the designated time period. The PGDT would then be connected to a computer by means of a dedicated port and would stream all of its information to the PM software housed in the computer. The data would now be translated into 3D imagery on a display panel.
The species of beam emitted by the BB would have the ability to pass through the contents of the small and large intestines as if invisible. The beam would have no harmful effect on any tissue even with repeated exposure to the same area. The PGDT unit, which is adhered to the skin of the patient’s abdomen, would emit a pulsed beam. When it reaches the surface of the BB it would trigger all of the ER’s to fire simultaneously and emit their scanning beams.
The PM software would calculate orientation. It would correlate the hits obtained and construct a section of the GIT representing the its internal topography. These sections would be pieced together digitally to form a seamless spatially accurate rendering of the system.
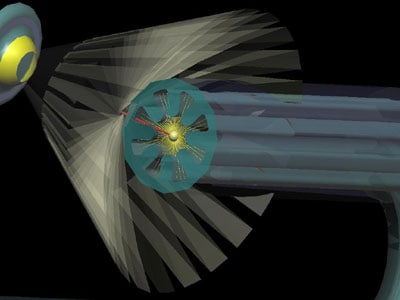
Images “Boehm 10,” “Boehm 11,” and “Boehm 12” are artistic representations of the PGDT unit and the BB engaged in data transfer with the BB inside the small intestine. Image “Boehm 13” is an artistic representation of the BB in scanning mode in sections of the small intestine. The Pixel Matrix software would center-correct for off-axis movement of the BB.
The BB device would be stored in a sterilized environment until ready for use to minimize any risk of infection. Due to the fairly rapid transit time (~2 days) from ingestion to elimination, chances of an immune response should be very low. After elimination, the BB will cease to function, as it requires the pulsed beams of the PGDT to activate it. The shell (as mentioned earlier) would be made of a biodegradable material and once degraded would release bonding holding all of the ER units in place. The ERs would separate becoming, in essence, harmless and non-functional micron sized particles that would be processed and disposed of along with all other solid waste.
The GMSD and system would serve as a useful, minimally invasive, biocompatible diagnostic tool for generating high-resolution 3D imagery of the gastrointestinal tract. It would be relatively simple to implement, minimize any chance of infection or discomfort, and the scanning would not be disruptive to the patient who could carry on with his/her normal affairs. Also, the GMSD would be environmentally friendly as the body of the internalized device (BB) would be made of a biodegradable material and degrade into smaller (micron sized) particles that could easily be treated and disposed of along with all other solid waste products.
The GMSD would be beneficial to physicians by providing a new and more precise method of imaging the GIT: It would aid them by offering more detailed information to apply to preventative care; it would assist them by acting as an accurate diagnostic tool; and it will increase the efficacy of their treatments.