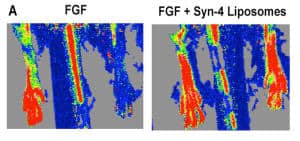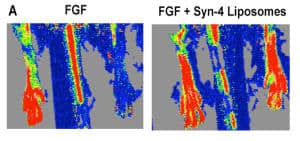
“Hindlimb ischemia was created in rats and treatments were delivered over seven days with an osmotic pump. The laser doppler imaging above shows the rat’s hind limb prior to treatment (on the left) and with increased blood flow (image on the right) just seven days after treatment.”
A major advantage of nanoparticles used in nanomedicine is that they can combine and deliver together more than one therapeutic component. This capability has been brought to bear in the quest to encourage regenerative blood vessel growth after ischemic disease, which causes much cardiovascular morbidity. Delivering a growth factor in a nanoparticle containing a different biomolecule as a coreceptor achieves results where delivering the factor alone had failed. A hat tip to ScienceDaily for reprinting this University of Texas at Austin news release “New Ability to Regrow Blood Vessels Holds Promise for Treatment of Heart Disease“:
University of Texas at Austin researchers have demonstrated a new and more effective method for regrowing blood vessels in the heart and limbs — a research advancement that could have major implications for how we treat heart disease, the leading cause of death in the Western world.
The treatment method developed by Cockrell School of Engineering Assistant Professor Aaron Baker could allow doctors to bypass surgery and instead repair damaged blood vessels simply by injecting a lipid-incased substance into a patient. Once inside the body, the substance stimulates cell growth and spurs the growth of new blood vessels from pre-existing ones.
The method has been tested successfully on rats, and findings of the study were published recently in the Proceedings of the National Academy of Sciences [abstract].
“Others have tried using growth factors to stimulate vessel growth in clinical trials and have not been successful,” said Baker, a faculty member in the school’s Department of Biomedical Engineering. “We think that a major reason for this is that previous methods assumed that the diseased tissues retained the ability to respond to a growth stimulus. Our method basically delivers extra components that can restore growth factor responsiveness to the tissue of patients with long-standing clinical disease.”
The ability to regrow blood vessels could prove crucial to treating chronic myocardial ischemia disease, which affects up to 27 million patients in the U.S. and leads to a reduction of blood flow in the heart and lower limbs — ultimately causing organ dysfunction and failure. …
The new method introduced by Baker and his research team builds on a promising revascularization approach that, up until now, has shown limited efficacy in clinical trials for treating human disease.
The method combines a growth factor — a substance capable of stimulating cellular growth, proliferation and cellular differentiation, as well as healing wounds — known as fibroblast growth factor 2 (FGF-2) with a lipid-embedded receptor to enhance its activity.
A challenge for scientists and engineers, however, has been getting FGF-2 to bind with cell receptors — the very molecules often found on the surface of the cell that receive chemical signals and direct activity in the cell from outside sources.
To overcome this, Baker’s method embeds the growth factors in synthetic lipid-based nanoparticles containing a coreceptor known as syndecan-4. The nanoparticles containing co-receptors that, when delivered with the growth factor, enable improved cell binding so that the growth factor can direct the targeted cell to divide, proliferate and form new cells for tissue regrowth.
The incased substance was injected into rats with hindlimb ischemia and stimulated a complete recovery from the ischemia in just seven days.
Mammalian cells are very complex mechanisms, and several decades of experience with biotechnology have demonstrated that newly discovered molecules expected to do great things often underperform expectations because changing a cell requires several molecules working together. Nanoparticles have the potential to be complex enough to accomplish what single molecules cannot.
—James Lewis, PhD